Each November, the New York E-health Collaborative, a nonprofit organization that serves as a public resource for health information technology in New York State, holds the annual Digital Health Conference that brings together hundreds of leaders from healthcare, entrepreneurship, venture capital, business, government and academia to discuss the trends, trials, and triumphs occurring in the field of healthcare meets technology. This year’s conference was held at Chelsea Piers in Manhattan.
This year’s keynote speakers included Dr. Eric Topol, practicing and renowned cardiologist, author of “The Creative Destruction of Medicine”, Director of the Scripps Translational Science Institute, and Chief Medical Advisor at AT&T, and Dr. Ezekiel Emanuel, Vice Provost for Global Initiatives and Chair of the Department of Medical Ethics and Health Policy at the University of Pennsylvania and Wharton, founding chair of the Clinical Center of the National Institutes of Health, and author of “Reinventing American Health”. Dr. Topol’s keynote highlighted several ideas and trends in the field of digital health including the democratization of medicine with the patient at its center (the shift from “the doctor will see you now to the PATIENT will see you now” and who holds information,”nothing about me without me”), its conduction as a digitized data science, our entry into an age of personalized medicine, genomics and digital tools (smartphone EMR’s and diagnostic plugins, mobile solutions for mental health and wellness, nanomedicine, embedded sensors, virtual visits) designed to provide value to users. Dr. Topol spoke about the patient’s room as the new hospital room in an age of de-centralized and distributed digital technology and the more central role that genomics needs to play in regards to diagnostics (“Cancer is a genomic disease, but we don’t diagnose it that way”, using genomics to unlock previously labeled “idiopathic disease” and the potential for molecular-level autopsy) and use in treatment, (some reactions to drugs are based on a person’s genetic makeup, i.e. the metabolism of the blood-thinner warfarin, and the value there is in knowing who will and won’t benefit from the drug before prescribing it). He also talked about the ballooning cost of healthcare, citing INC’s article, “The Trillion Dollar Cure”, and Elisabeth Rosenthal’s New York Time article “Paying til It Hurts”, and how technology can help save time and money (as an example, molecular sequencing of pathogen drug susceptibility vs. traditional culture methods means knowing if an antibiotic will work for a patient, in minutes vs. a few days -the time it usually takes cultures to grow).
Dr. Emanuel’s keynote focused on the impact that health information technology will have on re-inventing the healthcare system and its effects on the economy. He cited that in 2014, the United States will spend $3 trillion on healthcare, making it the world’s fifth largest economy. Chronic conditions account for 80% of that cost and much of it is spent in hospitals. “The American Health Care system has more than enough money, it’s a matter of how we use that money”. Dr. Emanuel outlined 6 megatrends in healthcare (1) The diffusion of VIP care for the chronically and mentally ill (providing tertiary team-based preventative care and telemedicine to decrease ER visits, re-admissions, falls, health-related costs) (2) The expansion of digital health medicine and the closure of hospitals (with a move towards digitally-enhanced LEAN-model outpatient facilities) (3) The end of insurance companies as we know them (replaced by accountable care organizations consisting of doctors, hospitals and other healthcare providers with value-based reimbursement replacing do-more-charge-more fee-for-service) (4) The end of employer-sponsored insurance (with a move towards people buying insurance from health exchanges) (5) The end of healthcare inflation and (6) The evolution of academic health centers (leading to a change in health education and delivery).
Day 1 of the general discussion sessions began with the presentation of the PATH (Promoting Enhancement of Technology in Healthcare) awards to Dr. Patricia A. Bomba, the Vice President and Medical Director of Geriatrics, Excellus BlueCross BlueShield for her work in developing a readily available MOLST (medical order for life-sustaining treatment) form which documents a patient’s preference for life-sustaining treatment and creating the eMOLST directory for New York, and Larry McReynold’s, President of Lutheran Family Health Centers, for his dedication to improving healthcare for the medically underserved in Brooklyn.
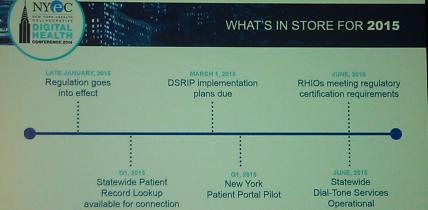
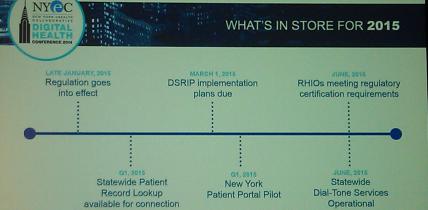
Next came, New York E-health Collaborative, Executive Director David Whitlinger’s presentation on the state of Health IT in New York, and what lies ahead in its digital road map. The SHIN-NY (Statewide Information Network of New York) is up and running in all 9 RHIO’s (Regional Health Information Organizations) in the state. 83% of hospitals, 56% of public health organizations, 35% of home care agencies and 14% of clinical practice sites (a complex web of connections given the number of providers in the state and in New York City alone) are connected. There are over 5 million MD to MD direct messaging transmissions a month and 6 million (about 1/3 of the state) New Yorkers have already granted their personal health care providers permission to share records via opt-in consent. Other 2014 accomplishments include the allocation of $55 million in state funding and $30 million in federal (CMS) funding for the SHIN-NY, New York State Department of Health licenses for Electronic Hospital Records, and RHIO’s poised for health information technology certification and provision of Dial-Tone service requirements (services that will provided free of charge, including: statewide patient record lookup inclusive of lab results and radiology reports, notify/alert/subscribe notifications, and public health reporting integration). The road map into 2015 includes the interconnection of the RHIO’s, the public and official launch of the statewide Patient Portal for New Yorkers (disclosure: I was involved in the design), and the use of federal and state allocated funds for projects that help the medically underserved.
Mr. Whitlinger also announced a new program that is a joint venture between HIMSS (Healthcare Information and Management Systems Society), IHE USA (Integrating Healthcare Enterprise, a nonprofit that drives adoption of standards-based interoperability), ICSA labs (an independent division of Verizon that tests platform security capabilities) and the EHR/HIE Interoperability workgroup (NYeC-led coalition of 19 states which represents about 50% of the U.S. population, 20 EHR vendors and 22 HIE vendors) designed to make data sharing between organizations, states and health IT systems easier, thus helping to lower healthcare costs and improve outcomes.
Day 2 of the general sessions featured sessions on sensors, the use of data in athletics and a demo of brain-sensing technology. Dr. Alan Greene, Chief Medical Officer of Scanadu (a consumer medical device company in the running for creating an XPRIZE tricorder) spoke about science, sensors and superpowers. Having medical technology can be likened to having a super power (i.e. X-rays to see through the body, a power held by Superman) and today’s innovative technology make it even more possible to be superheroes. However, Dr. Greene cautioned, in quoting Spider Man lore, ” with great power comes great responsibility”.
In his talk, “Data Not Doping, How the Women’s Cycling Team Beat All the Odds at the 2012 London Olympics”, Sky Christopherson, Olympic athlete and co-founder of OAthlete, talked about using the power of data in helping the underdog women’s U.S. track cycling team win their first gold medal in 20 years, in a year that the men’s cycling team withdrew due to the Lance Armstrong doping scandal . The underfunded team relied on friends and family, as well as health hacking, using blood work, quantified self measures, combined with coaching to take the gold -a story that will be captured in the upcoming film, “Personal Gold”.
In “Out of the Lab and Into the World”, Ariel Garten, co-founder and CEO of InteraXon spoke about brain-sensing device Muse (designed to improve cognition and reduce stress), and its use in mental health. She also spoke of her experiences working with consumer brain tech, using the mind to create concerts or even levitate a chair.
This year’s breakout sessions included discussions on wearable technology, interoperability and coordinated care in a connected future, ethical policy on the use of consumer health data, the hype and hope of Big Data on the road to personalized medicine, data sharing on health information exchanges, and connected health around the world, as well as a Patient Shark Tank that featured patient panelists who assessed digital health companies, featuring Board Rounds (a service that enables post-discharge care after an ER visit), Canopy (language assistance tools to benefit patients and providers), SMAART (Show Me Again, All Recommended Treatments-which utilizes Google Glass technology to automatically record significant healthcare interactions), and the winners, a tie between Nutrify (a web and mobile-based application that changes how patient education on diet is done post-discharge) and Clear Health Costs (a cost transparency tool that people can search to look up prices for medical procedures and items).
The DSRIP (Delivery System Reform Incentive Payment Program) panel discussed the goal of reducing avoidable hospital admissions by up to 25% over 5 years and strengthening the safety net using $6 billion out of $8 billion in federal savings generated by the Medicaid Reform team. The program requires networks of PPS (Performing Provider Systems) to work together to deliver population-based care in projects that use data analytics, improved communication and patient care to New York’s Medicaid beneficiaries and the uninsured. More information on the program can be found here: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/
A panel featuring Brian O’connor, Chair of the European Connected Health Alliance, Millard Chang, China Connected Health Alliance (along with ECHA, represents a market of over 2 billion people across 2 continents) and Chair of Pegasus Holdings Group, Julien Venne, Strategic Advisor and European Project Team Leader, European Health Alliance, and Dave Whitlinger, the Director of the New York E-health Collaborative, discussed the different political, tax, policy and care infrastructures of China, Europe and the United States. Despite these differences, they face similar challenges including aging populations and decreasing a labor force, the need for Big Data, analytics and better care coordination, and growing healthcare costs. They also discussed the opportunity there is in connecting networks, learning from each other and sharing markets.
This year’s exhibitors at the conference featured an innovation showcase by the California Healthcare Foundation on digital health companies across the globe, UK Technology Trade Investment, Invest North Ireland, asthma-focused tech company Propeller Health, and the Muse wearable as well as other companies that span the field of digital health.
2014 has been a blockbuster year for digital health, with notable IPO’s, the rise of investment in HIT companies, changes in government policy, innovative initiatives at healthcare institutions and healthcare-focused corporations, and 2015 looks like it will build upon that and continue this upward and progressive trend.
Don’t want to miss the next awesome NYC event like this one? Visit the AlleyWatch NYC Tech and Startup Event calendar by clicking the banner below: